318 JOURNAL OF COSMETIC SCIENCE consumer products under comparable, controlled conditions. The purpose of this inves tigation was to examine ocular irritancy levels elicited in human subjects by various categories of a specific class of cosmetic and consumer products that have a potential to enter the eye inadvertently during use. MATERIALS AND METHODS SUBJECTS AND MATERIALS The results from 205 human subjects (410 eyes) with normal, non-contact-lens-wearing eyes, ranging in age from 19 to 69 years, were reviewed from 12 ocular instillation studies. All subjects were instructed not to wear any eye makeup for their pre-test qualifying ophthalmic examination. Prior to enrollment, all inclusion/exclusion criteria were verified, an informed consent form was obtained, and a medical history was taken. The test materials assessed, which were provided by multiple clients, belonged to one of seven categories (Table I), which included liquid makeup (9.76%), shampoo (39.02%), baby wash (19.51 %), eye makeup remover (14.63%), mascara (2.44%), powder eye shadow (9.76%), and facial cleanser (4.88%). PROCEDURE OF ACUTE INSTILLATION Each subject was reclined in an automated ophthalmic chair (Isell/Diversatronics, Inc.) at a 60° angle. A 75-100-µl or 30-mg dose of each test material was instilled into the inferior cul de sac, while the lower eyelid was retracted downward. Each test material was instilled in the right or left eye, in rapid sequence. Any excess tearing resulting from the instillation was gently blotted, with a separate tissue used for each eye. Ophthalmic examinations were performed at 30 seconds, 5 minutes, 15 minutes, 60 minutes, 120 minutes, and 24 hours post-instillation. During the course of the study, subjects re mained in a controlled environment to preclude exposure to any external factors that could influence the evaluation of the test material (i.e., rubbing of eyes, smoke, bright lights, etc.). OPHTHALMIC EXAMINATION The ophthalmic evaluation included assessments of subjective reports of ocular symp toms, objective ophthalmic irritation, and ocular surface fluorescein staining. Subjective Products Liquid makeup Shampoo Baby wash Eye makeup remover Mascara Powder eye shadow Facial cleanser Total Table I Distribution of Product Types Preparation Number of eyes Neat 40 10% 160 Neat 80 Neat 60 Neat 10 Neat 40 Neat 20 410 % 9.76 39.02 19.51 14.63 2.44 9.76 4.88 100.00
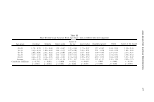
ASSESSMENT OF OCULAR IRRITANCY 319 irritation was determined by ascertaining from the subject any experiences of ophthalmic irritation (i.e., stinging, burning, itching, dryness, and/or foreign body sensation) at the time of the specified examination. Subjects were examined for evidence of excessive lacrimation. Each subject's upper and lower eyelids, specifically the lid margins, were examined for evidence of redness, scaling, swelling, and/or excessive secretions of the meibomian gland orifices. The palpebral and bulbar conjunctivae were examined and scored for redness, inflammation, and follicular and/or papillary reactions. The cornea was examined for evidence of any neovascularization, edema, infiltrates, opacities, and/or epithelial defects. To assess fluorescein staining patterns, a Fluorets sterile ophthalmic strip (fluorescein sodium BP, Smith & Nephew) was inserted into the inferior cul de sac of each eye after a small amount of Dacriose sterile irrigating solution had been dropped onto the Fluorets® strip. The integrity of the palpebral and bulbar conjunctivae, corneal epithelium, and caruncle were then evaluated with a Haag-Streit Bern model Z 2982A slit lamp biomicroscope, and the tear film break-up time was assessed. DATA ANALYSES The grading scale, designed by Bruce E. Kanengiser (3), for all parameters was 0--4 (0 = normal, 1 = trace, 2 = mild, 3 = moderate, and 4 = severe), with the exception of fluorescein ophthalmic staining, in which a 14-point scale was employed to evaluate the integrity of the palpebral and bulbar conjunctivae, corneal epithelium, and caruncle (Table II). Additionally, tear film break-up time was assessed by determining the time that elapsed before the first hole (dry spot) appeared in the corneal fluorescein layer(::::::10 seconds is normal). Microsoft Excel (2000) and SigmaStat/SigmaPlot Version 5 were used to compile and statistically analyze the data. Student's t-test and ANOV A and correlation (r-value) tests were performed. Statistical significance was declared for all Table II Palpebral and Bulbar Conjunctival, Caruncular, and Corneal Fluorescein Ophthalmic 14-Point Area Staining Scale (3) Ocular irritancy No ocular irrirancy Mild ocular irritancy range Moderate ocular irri tancy range Severe ocular irritancy range Level 0 2 3 4 5 6 7 8 9 10 11 12 13 Description (% staining in quadrant) No staining 0 and ::=:::10% 10% and ::=:::20% 20% and :2::30% 30 and ::=:::40% 40% and ::=:::so% 50% and :2::60% 60% and ::=:::70% 70% and ::=:::so% 80% and :2::90% 90% and :2::100% Mild superficial tissue abrasion Moderate superficial tissue abrasion Severe superficial tissue abrasion Density grading scale: 1 = occasional, scattered punctate staining 2 = more uniform pattern of diffusely scattered punctate staining 3 = dense foci of punctate staining within the areas of diffuse punctate staining 4 = general pattern of dense punctate staining.
Purchased for the exclusive use of nofirst nolast (unknown) From: SCC Media Library & Resource Center (library.scconline.org)